CORNEA
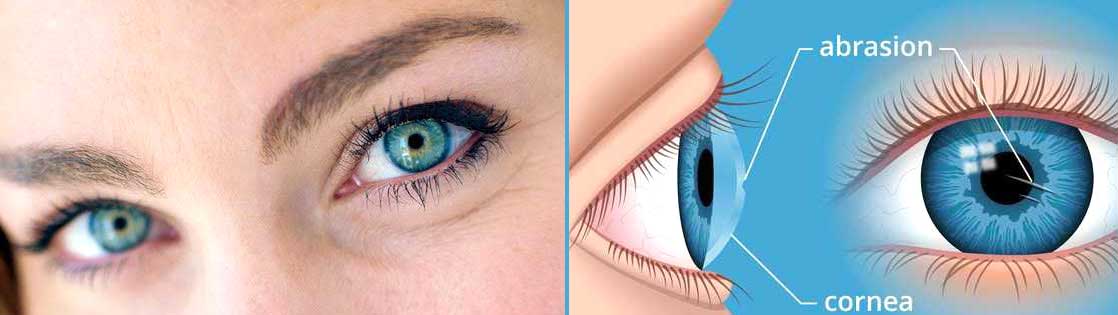
CORNEA
CORNEAL TRANSPLANTS
WHAT IS A CORNEAL TRANSPLANT?
With corneal transplants, scarred or damaged tissue is replaced with healthy donor tissue. Corneal transplants either replace the whole cornea (standard full thickness known as Penetrating Keratoplasty) or individual layers (partial thickness known as DSAEK, DMEK and DALK). The type of transplant performed depends on the prior condition and extent of the damage.
INDICATIONS FOR FULL THICKNESS CORNEAL TRANSPLANTS
- Advanced keratoconus with severe scarring
- Severe Herpetic scarring
- Full thickness traumatic injury
- Full thickness corneal scar due to any reason
INDICATIONS FOR DALK
- Keratoconus, corneal scarring & pellucid marginal degeneration
- Stromal Corneal Dystrophies
- A healthy endothelium (the innermost layer of the cornea)
INDICATIONS FOR DSAEK / DMEK/PDEK
- Fuchs’ dystrophy or other endothelial dystrophies
- Corneal failure after cataract, glaucoma or retinal surgery
- Endothelial failure or rejection of a full thickness transplant
Who Is Candidate?
DSAEK PROCEDURE
Recovery Time
In most cases, the vision will begin to improve in about one week. Full recovery is typically 3 months.
BENEFIT FROM A CORNEAL TRANSPLANT?
When the retina, optic nerve and lens are healthy and the only cause for defective vision is a hazy cornea preventing the light to form image on the retina, then corneal transplant has a very good prognosis depending on other comorbid factors. Chances of corneal transplant rejection in a body is much less than any other organ transplantation in the body as HLA matching is not required.
HOW IS THE SURGERY PERFORMED?
Corneal transplants are generally done under local anaesthetic. With full thickness transplants, the damaged cornea is removed through a process called trephination and replaced with a donor cornea. The transplant is then secured using tiny stitches. Partial thickness transplants replace only certain layers, leave the rest intact and use fewer stitches. On treatment day, you will be instructed to arrive at the hospital about 1.5 hours in advance and the surgery will take approximately 30 minutes. No overnight hospital stay is required.
WHAT ARE THE POSSIBLE COMPLICATIONS?
The success rate of corneal transplants has drastically improved in the last 30 years. Today, the overall success rate is above 85%. However, it can vary from 50% to 95% depending on the condition being treated.
Corneal transplants remain a serious surgery with certain risks that you should be aware of. The primary risks are rejection and infection which are minimized with the use of antibiotic and steroid drops. Other less common complications include bleeding, swelling, glaucoma and retinal detachment. Fortunately, the majority of complications are treatable and have good outcomes.

HOW LONG IS HEALING TIME?
Healing time is different for everyone. You can expect to have moderate discomfort, irritation and redness for up to 3 weeks. Best possible vision is achieved once wounds have fully healed and stitches removed. Healing of a full thickness transplant can take up to 1 year. Visual improvement with DMEK and DSAEK usually occurs in a few weeks.
WHAT DO I NEED TO DO BEFORE AND AFTER SURGERY?
- 1. You should ensure that you understand all instructions provided.
- 2. Starting antibiotics drops 2 days prior to surgery and continue as per the prescription.
- 3. You will also take steroid drops that will be gradually reduced over time in tapering doses.
- 4. It is essential to take your drops as prescribed to maintain function of the transplant for a long period with regular follow ups.
- 5. After surgery you should avoid any heavy lifting and strenuous activity for 1 month.
PTERYGIUM

Pterygium is a veil like lesion that usually occurs in exposed part of white of the eye. This grows slowly over the cornea (the central black portion) and can obstruct vision or deteriorate vision by inducing cylindrical power.
Symptoms Of Pterygium May Include:
- Burning
- Gritty feeling
- Itching
- Sensation of a foreign body in the eye
- Blurred vision
Causes Of Pterygium : Significant Risk Factors Include:
- Prolonged exposure to ultraviolet light
- Dry eye
- Irritants such as dust and wind
Treatment Of Pterygium
Pterygium is not only cosmetically disfiguring but can affect the vision also. In view of this it is advisable to surgically excise it at the earliest. Surgical excision of pterygium is a simple day care procedure with no adverse effects
Latest surgery method involves removing the pterygium tissue and placing a healthy tissue on bare area which prevents recurrence and is cosmetically very rewarding.
Surgery for pterygium is minimally invasive, sutureless and is very safe.
Pterygium does not respond to medical treatment of any kind be it in form of eye drops or ointment and surgical excision is the treatment of choice.