RETINA SERVICES
Diseases and conditions of the retina
- Age-Related Macular Degeneration
- Diabetic Retinopathy
- Retinal tear
- Retinal Detachment
DIABETIC RETINOPATHY:
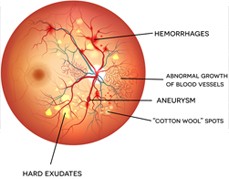
The cells in persons with diabetes mellitus have difficulty using and storing sugar properly. When blood sugar gets too high, it can damage the blood vessels in the eyes. This damage may lead to diabetic retinopathy.
TYPES OF DIABETIC RETINOPATHY:
- Background or nonproliferative diabetic retinopathy - blood vessels in the retina are damaged and can leak fluid or bleed. This causes the retina to swell and form deposits called exudates.
- Many patients may not notice any change in their vision when they develop this early form of the disease, but it can lead to other more serious forms of retinopathy that severely affect vision. Fluid collecting in the macula is called macular edema and may cause difficulty with reading and other close work.
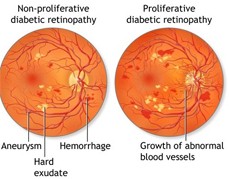
PROLIFERATIVE DIABETIC RETINOPATHY:
- New, fragile blood vessels grow on the surface of the retina. These new blood vessels are called neovascularization, and can lead to serious vision problems, because the new vessels can break and bleed into the vitreous. When the vitreous becomes clouded with blood, light is prevented from passing through the eye to the retina.
- This can blur or distort vision and frequently causes sudden and severe loss of vision. The new blood vessels can also cause scar tissue to develop, which can pull the retina away from the back of the eye. This is known as retinal detachment, and can lead to blindness if untreated. In addition, abnormal blood vessels can grow on the iris (the colored part in the front of the eye), which can lead to severe glaucoma.
TREATMENT OF DIABETIC RETINOPATHY:
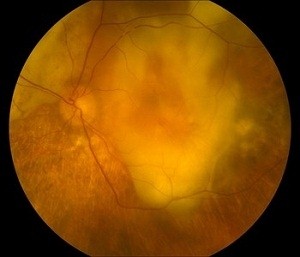
 Good control of diabetes with intensive management and control of blood sugar will delay, and possibly prevent, both the development and progression of diabetic retinopathy. Patients with diabetic retinopathy frequently need to have special photographs of the retina taken. This series of photos is called fluorescein angiography.
Good control of diabetes with intensive management and control of blood sugar will delay, and possibly prevent, both the development and progression of diabetic retinopathy. Patients with diabetic retinopathy frequently need to have special photographs of the retina taken. This series of photos is called fluorescein angiography.
- Laser Photocoagulation is one of the most common treatments for diabetic retinopathy. Focal photocoagulation consists of laser directed at the retina to seal leaking blood vessels in patients with background diabetic retinopathy. Panretinal photocoagulation consists of laser spots scattered through the sides of the retina to reduce abnormal blood vessel growth (neovascularization) and help seal the retina to the back of the eye in patients with proliferative diabetic retinopathy. This can help prevent retinal detachment.
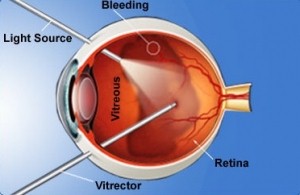
- Vitrectomy Surgery is performed for patients with very advanced proliferative diabetic retinopathy or retinal detachment. In vitrectomy, the surgeon removes the blood-filled vitreous and replaces it with a clear solution. This allows light to pass through the clear fluid to the retina, where the images are conveyed to the brain.
- These involve intravitreal injections of small amounts of medication into the eye
Age-Related Macular Degeneration
What causes in AMD?
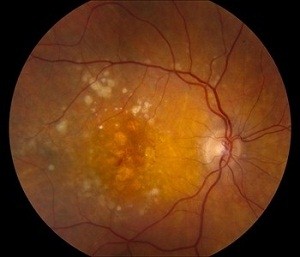
During normal aging, yellowish deposits, called drusen, form under the retina, which is the light-sensitive layer of tissue at the back of the eye that provides clear, sharp images.
As drusen increase in size and number, they can interfere with proper functioning of the retina, damaging or killing the light-sensitive cells of the macula.
Because the macula’s light-sensitive cells provide the ability to have sharp, detailed vision, the results can be blurring of central vision and a devastating impact on the ability to enjoy activities of daily life, such as reading, driving, or even recognizing the face of a friend or family member.
This form of age-related macular degeneration is called dry AMD. Dry AMD can be a precursor to wet AMD.
 Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These blood vessels often leak blood and fluid, damaging or killing light-sensitive cells—loss of vision occurs quickly.
Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These blood vessels often leak blood and fluid, damaging or killing light-sensitive cells—loss of vision occurs quickly.
Although approximately 80 percent of patients with age-related macular degeneration have dry AMD, wet AMD is responsible for 80 to 90 percent of severe loss of vision with this disease.
Risk factors
Many people ask if age-related macular degeneration can be prevented. Like most things in life, there is no easy answer.
The primary risk factor for AMD is age—the older you are, the greater your risk. Also, people with a family history of AMD are at higher risk, as are women and people of European descent.
Lifestyle factors increasing risk for AMD:
- Cigarette smoking
- Obesity
- Hypertension (high blood pressure)
- Excessive sun exposure
- Diet deficient in fruits and vegetables
Dry AMD symptoms
- Need for brighter light when reading
- Difficulty adapting to low light levels
- Increased blurriness of printed words
- Decrease in brightness of colors
- Blurred spot in the center of the field of vision
- Blank or black spot in the field of vision (spot will start small and grow over time, possibly leading to blindness
Wet AMD
Early stage wet AMD
End stage wet AMD with scarring
Wet AMD Symptoms
- Sudden painless decline in central vision
- Visual distortions, such as straight lines appearing wavy, or objects appearing larger or smaller than they are
- Well-defined blind spot in the center of vision
It is important to pay close attention to any decline in central vision—both near and distant.
Diagnostic Tests
Dilated eye exam
In this examination, a physician uses eye drops to dilate, or widen, the pupil to examine the retina. Regular dilated eye exams are important, especially for those who are at a higher risk for developing AMD.
If you are over age of 50, it is a good idea to schedule a periodic eye examination to look for the earliest signs of AMD before any vision loss has occurred.
Ocular coherence tomography
The physician may suggest an optical coherence tomography (OCT) exam. This test provides cross-sectional images of the retina that show its thickness, helping determine whether fluid has leaked into retinal tissue and other changes that happen with AMD.
Amsler grid
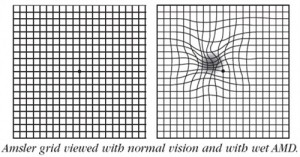 Another way to detect AMD is by using an Amsler grid test. In this test, the patient covers one eye at a time and stares at the black dot at the center of the grid. If the straight lines appear broken, crooked, wavy, bent, or distorted, the patient may have AMD.
Another way to detect AMD is by using an Amsler grid test. In this test, the patient covers one eye at a time and stares at the black dot at the center of the grid. If the straight lines appear broken, crooked, wavy, bent, or distorted, the patient may have AMD.
It is important to note that this test is hardly sufficient to rule out the possibility of AMD, as many people with the disease may see no abnormalities on an Amsler grid.
Visual acuity test
Because AMD affects visual acuity, an eye chart can also be an indicator of the development of AMD.
Treatment and drugs
There is no known cure for AMD, but early detection and proper treatment can protect vision from further deterioration.
Dry AMD treatments
- Currently, no medical treatments exist for dry AMD, but the retina specialist will suggest strategies to slow its progression—taking vitamin or mineral supplements, for example.
- If you have Dry AMD, it is extremely important to follow your retina specialist’s eye examination schedule.
- Biweekly Amsler’s grid self-examination
- Also, if you experience new symptoms or your notice any deterioration in vision, see your retina specialist right away.
Wet AMD treatments
There is a variety of medical treatments that can help stop further vision loss caused by wet AMD:
- Laser surgery – These procedures can eliminate abnormal blood vessels and prevent additional leakage, bleeding, or growth.
- Photodynamic therapy – In this treatment, the patient is injected in the arm with a medicine that is triggered by a laser to destroy abnormal blood vessels.
- Eye injections – These medicines destroy abnormal blood vessels in the eye and prevent them from leaking.
Intravitreal Injections
- Pegaptanib (Macugen)
- Bevacizumab (Avastin)
- Ranibizumab (Lucentis): Is the newest and most effective anti-VEGF agent approved by the FDA for the treatment of wet age-related macular degeneration (AMD).
FLASHES & FLOATERS:
Some people may occasionally see small specks or clouds moving in your field of vision. These are called floaters. Floaters are actually tiny clumps of gel or cells inside the vitreous , the clear jelly-like fluid that fills the inside of the eye. While these objects look like they are in front of the eye, they are actually floating inside. When people reach middle age, the vitreous gel may start to thicken or shrink, forming clumps or strands inside the eye. The vitreous gel pulls away from the back wall of the eye, causing a posterior vitreous detachment. Posterior vitreous detachment is more common in people who:
- Are near-sighted
- Have undergone cataract operations
- Have had YAG laser surgery of the eye
- Have had inflammation inside the eye
When the vitreous shrinks, it tugs on the retina, creating a sensation of flashing lights. The flashes of light can appear off and on for several weeks or months. As we grow older, it is more common to experience flashes.
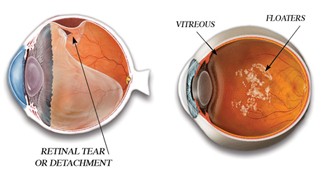
As the shrinking vitreous gel pulls away from the wall of the eye, it can cause a retinal tear in places where the vitreous gel sticks too tightly to the retina. This sometimes causes a small amount of bleeding in the eye that may appear as new floaters. A torn retina is always a serious problem, since it can lead to a retinal detachment.
RETINAL DETACHMENT
What is a retinal detachment?
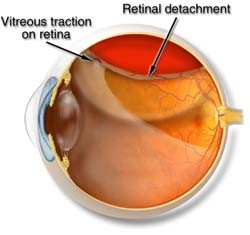 As the vitreous gel in the back of the eye starts to liquefy, it can separate from the retina, a condition called vitreous detachment. If the vitreous gel adheres too firmly to the retina, a retinal tear can occur with a vitreous detachment. A retinal detachment occurs when fluid leaks through the tear and separates the retina from the back of the eye.
As the vitreous gel in the back of the eye starts to liquefy, it can separate from the retina, a condition called vitreous detachment. If the vitreous gel adheres too firmly to the retina, a retinal tear can occur with a vitreous detachment. A retinal detachment occurs when fluid leaks through the tear and separates the retina from the back of the eye.
Symptoms
Patients may have Flashes and floaters as their first symptoms. Patients may describe a "curtain" being drawn across the peripheral vision or decreased peripheral vision. If untreated, most retinal detachments will cause progressive loss of vision and eventually total blindness.
Treatment for Retinal Detachment:
- Laser Treatment of the Retina : Laser is usually performed to decrease leakage in the retina, treat abnormal blood vessel growth, or create a beneficial scarring effect that can help prevent a retinal detachment. It is a non invasive procedure .
- Scleral Buckle : This treatment for retinal detachment involves surgically sewing a silicone band (buckle) around the white of the eye (called the sclera) to push the sclera toward the tear until the tear heals. This band is not visible and remains permanently attached. Laser or cryo treatment may then be necessary to seal the tear.
- Vitrectomy : A sophisticated microsurgical technique in which the vitreous gel is removed from inside the eye with a small, specialized cutting device, an operating microscope to look into the eye, and microsurgical instruments.
- Depending on the complexity of the retinal detachment, various combinations of vitrectomy, buckle, laser and gas bubble may be used to repair the retina
Specialisation
- Lasik / Refractive Surgeries
- Cornea
- Cataract
- Keratoconus
- Retina Surgery
- Glaucoma Services
- Oculoplastic Surgery
Contact Information
Dr. Shaila Rajkumar Patel
MBBS, DNB Ophthal (Arvind Eye Hospital), F.C.R.S. (Fellowship in Cornea and Refractive Surgery), Fellowship in Advanced Phaco, MNAMS
301, 3rd Floor, MTNL Road, Near Don Bosco School, Mira Road (East), Thane - 401 107
+91 83698 81371